Endometriosis is a chronic health condition that affects millions of women worldwide, often causing pain, discomfort, and fertility challenges. Despite its prevalence, it remains widely misunderstood and is sometimes misdiagnosed, leading to delayed treatment and unnecessary suffering.
What is Endometriosis?
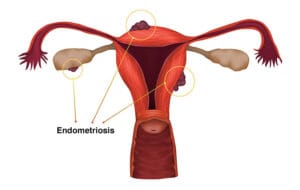
Endometriosis occurs when tissue similar to the lining of the uterus (endometrium) grows outside the uterus. These growths can develop on the ovaries, fallopian tubes, pelvic lining, and in some cases, even beyond the pelvic area.
Just like normal uterine lining, these misplaced tissues thicken, break down, and bleed during the menstrual cycle. However, because they have no way to exit the body, this can cause inflammation, scarring, and the formation of painful cysts called endometriomas.
Causes of Endometriosis
The exact cause is still not fully understood, but researchers believe several factors may contribute:
Retrograde menstruation – Menstrual blood flows backward into the pelvic cavity instead of leaving the body.
Genetic predisposition – A family history of endometriosis increases the risk.
Hormonal imbalances – High levels of estrogen may stimulate abnormal tissue growth.
Immune system disorders – A weakened immune response may fail to destroy misplaced endometrial cells.
Common Symptoms
Symptoms vary from person to person, and some women may have no symptoms at all. The most common include:
Severe menstrual cramps (dysmenorrhea)
Pain during or after sex (dyspareunia)
Painful bowel movements or urination during menstruation
Heavy or irregular menstrual bleeding
Chronic pelvic pain
Difficulty getting pregnant (infertility)
Fatigue, bloating, nausea
How is Endometriosis Diagnosed?
Diagnosis can be challenging because symptoms overlap with other conditions like pelvic inflammatory disease or ovarian cysts.
Pelvic exam – Checking for abnormalities.
Ultrasound or MRI – Imaging tests to detect cysts or tissue growths.
Laparoscopy – A minor surgical procedure that allows direct visualization and biopsy; this is the gold standard for diagnosis.
Treatment Options
While there is no known cure, treatments can help manage symptoms and improve quality of life. Options include:
1. Medication
Pain relievers (NSAIDs) to reduce discomfort.
Hormonal therapy to slow tissue growth (birth control pills, hormonal IUDs, GnRH agonists).
2. Surgery
Laparoscopic excision or ablation to remove or destroy endometrial growths.
Hysterectomy (removal of the uterus) in severe, treatment-resistant cases.
3. Lifestyle & Supportive Care
Diet changes (anti-inflammatory foods, reduced caffeine and processed sugar).
Regular exercise and stress management techniques like yoga or meditation.
Support groups or counseling for emotional well-being.
Impact on Fertility
Endometriosis is a leading cause of infertility, affecting up to 30–50% of women who struggle to conceive. However, with early detection and proper treatment, many women can still achieve pregnancy naturally or with assisted reproductive techniques like IVF.
Living with Endometriosis
Endometriosis is more than just “bad
periods.” It can impact work, relationships, mental health, and overall quality of life. Early diagnosis, effective management, and emotional support are essential to living well with this condition.
Bottom line: If you experience severe menstrual pain, heavy bleeding, or pelvic discomfort that interferes with daily activities, don’t ignore it. Consult a gynecologist for evaluation—early intervention can make a significant difference.


